
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Articles
- Cardiovascular Risk/Epidemiology
- Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
- Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):45-58. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0344

- 3,040 View
- 263 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are no clear data to support the cardiovascular (CV) risk categories and low-density lipoprotein cholesterol (LDL-C) treatment goals in Korean people with type 2 diabetes mellitus (T2DM). We evaluated the incidence of cardiovascular disease (CVD) according to comorbidities and suggested LDL-C treatment goals in Korean people with T2DM in nationwide cohort data.
Methods
Using the Korean National Health Insurance Service database, 248,002 people aged 30 to 90 years with T2DM who underwent routine health check-ups during 2009 were included. Subjects with previous CVD were excluded from the study. The primary outcome was incident CVD, defined as a composite of myocardial infarction and ischemic stroke during the follow-up period from 2009 to 2018.
Results
The mean age of the study participants was 59.6±10.9 years, and median follow-up period was 9.3 years. CVD incidence increased in the order of DM duration of 5 years or more (12.04/1,000 person-years), hypertension (HT) (12.27/1,000 personyears), three or more CV risk factors (14.10/1,000 person-years), and chronic kidney disease (18.28/1,000 person-years). The risk of incident CVD increased linearly from an LDL-C level of ≥70 mg/dL in most patients with T2DM. In T2DM patients without HT or with a DM duration of less than 5 years, the CVD incidence increased from LDL-C level of ≥100 mg/dL.
Conclusion
For primary prevention of CVD in Korean adults with T2DM, it can be helpful to lower LDL-C targets when there are chronic kidney disease, HT, a long duration of diabetes mellitus, or three or more CV risk factors. -
Citations
Citations to this article as recorded by- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Significant Gap Between Guidelines and Practice in the Management of LDL Cholesterol: Insight From the Survey of the Korean Society of Myocardial Infarction
Sang Yeub Lee, Kyung Hoon Cho, Jang Hoon Lee, Young Joon Hong, Jin yong Hwang, Myung Ho Jeong, Weon Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef
- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
- Cardiovascular Risk/Epidemiology
- Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
- Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):59-71. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0320

- 2,816 View
- 226 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To validate the treatment target of low-density lipoprotein cholesterol (LDL-C) level according to the cardiovascular disease (CVD) risk which was recommended by Korean dyslipidemia guideline.
Methods
We used the Korean National Health Insurance Service database which included 3,958,048 people aged 20 to 89 years who underwent regular health screening. The primary outcome was incident CVD, defined as a composite of myocardial infarction and stroke during the follow-up period from 2009 to 2018.
Results
The risk of CVD increased from LDL-C level of 70 mg/dL in very high-risk and high-risk groups and from 130 mg/dL in moderate-risk and low-risk groups. Adjusted hazard ratios (HRs) of LDL-C ranges 70–99, 100–129, 130–159, 160–189, and ≥190 mg/dL were 1.20 (95% confidence interval [CI], 1.08–1.33), 1.27 (1.15–1.42), 1.39 (1.23–1.56), 1.69 (1.45–1.96), and 1.84 (1.49– 2.27) in very high-risk group, and 1.07 (1.02–1.13), 1.16 (1.10–1.21), 1.29 (1.22–1.36), 1.45 (1.36–1.55), and 1.73 (1.58–1.90) in high-risk group. Adjusted HRs (95% CI) of LDL-C ranges 130–159, 160–189, and ≥190 mg/dL were 1.15 (1.11–1.20), 1.28 (1.22– 1.34), and 1.45 (1.36–1.54) in moderate-risk group and 1.07 (1.02–1.13), 1.20 (1.13–1.26), and 1.47 (1.37–1.57) in low-risk group.
Conclusion
We confirmed the incidence of CVD was increased in higher LDL-C range. The risk of CVD increased from ≥70 mg/dL of LDL-C in very high-risk and high-risk groups, and from ≥130 mg/dL of LDL-C in moderate-risk and low-risk groups in Korean adults. -
Citations
Citations to this article as recorded by- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
Byung Jin Kim, Kwang Soo Cha, Wook Hyun Cho, Eung Ju Kim, Seung-Hyuk Choi, Moo Hyun Kim, Sang-Hyun Kim, Jun-Bean Park, Seong-Mi Park, Il Suk Sohn, Kyu Hyung Ryu, In-Ho Chae
Journal of Cardiovascular Pharmacology and Therapeutics.2023;[Epub] CrossRef
- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
- Drug/Regimen
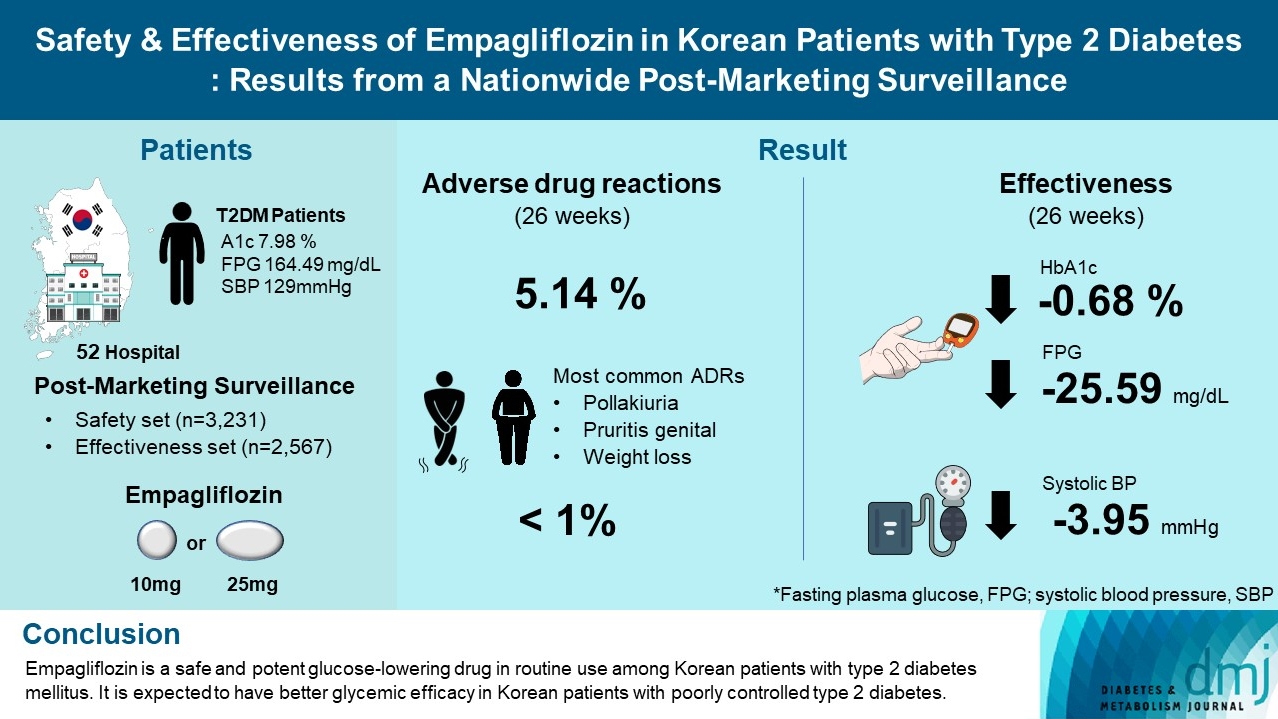
- Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
- Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
- Diabetes Metab J. 2023;47(1):82-91. Published online June 20, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0356
- 6,064 View
- 297 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To evaluate the safety and effectiveness of empagliflozin in routine clinical settings, we collected and assessed the clinical profiles of Korean patients with type 2 diabetes mellitus.
Methods
This was a post-marketing surveillance study of empagliflozin 10 and 25 mg. Information on adverse events and adverse drug reactions (ADRs) was collected as safety data sets. Available effectiveness outcomes, including glycosylated hemoglobin (HbA1c) level, fasting plasma glucose, body weight, and blood pressure, were assessed.
Results
The incidence rate of ADRs was 5.14% in the safety dataset (n=3,231). Pollakiuria, pruritis genital, and weight loss were the most common ADRs. ADRs of special interest accounted for only 1.18%, and there were no serious events that led to mortality or hospitalization. In the effectiveness data set (n=2,567), empagliflozin significantly reduced the mean HbA1c level and body weight during the study period by –0.68%±1.39% and –1.91±3.37 kg (both P<0.0001), respectively. In addition, shorter disease duration, absence of dyslipidemia, and higher baseline HbA1c levels were identified as the clinical features characteristic of a “responder” to empagliflozin therapy.
Conclusion
Empagliflozin is a safe and potent glucose-lowering drug in routine use among Korean patients with type 2 diabetes mellitus. It is expected to have better glycemic efficacy in Korean patients with poorly controlled type 2 diabetes mellitus. -
Citations
Citations to this article as recorded by- Evaluation of Efficacy and Safety of Empagliflozin in Bangladeshi Patients with Type 2 Diabetes Mellitus (EFFISAEM Study)
Mohammad Saifuddin, Ajit Kumar Paul, Sultana Marufa Shefin, Md. Jahangir Alam, Shahjada Selim, Sunjida Islam, Tanjina Hossain, Sadiqa Tuqan, Nusrat Sultana, Marufa Mustari, Ramen Chandra Basak, Kazi Ali Aftab, Indrajit Prasad, Mohammad Rafiq Uddin, Shoma
Indian Journal of Endocrinology and Metabolism.2024;[Epub] CrossRef - Comparison of the Pharmacokinetics, Safety, and Tolerability of Two Empagliflozin Formulations in Healthy Korean Subjects
Xu Jiang, Sungyeun Bae, Deok Yong Yoon, Shin Jung Park, Jaeseong Oh, Joo-Youn Cho, Kyung-Sang Yu
Drug Design, Development and Therapy.2023; Volume 17: 2137. CrossRef - Comparative safety of different sodium-glucose transporter 2 inhibitors in patients with type 2 diabetes: a systematic review and network meta-analysis of randomized controlled trials
Chun Xing Li, Li Yan Liu, Chen Xiao Zhang, Xu Hua Geng, Si Meng Gu, Yu Qiao Wang, Hua Liu, Qing Xie, Shuo Liang
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Evaluation of Efficacy and Safety of Empagliflozin in Bangladeshi Patients with Type 2 Diabetes Mellitus (EFFISAEM Study)

 KDA
KDA
 First
First Prev
Prev





